1 Apr, 2025 | Jennifer LaCoe PharmD, BCPS | No Comments
Prior Authorization: The April Fool’s Day Prank No One Laughs At

Prior authorizations can feel like a bad April Fool’s Day prank.
When you think you are getting the medication that can help your problem, your insurance has other ideas—prior authorization required. You ask how much and nearly pass out. Now, your doctor is left dealing with paperwork as you wait through the delay with frustration. You wonder if the approval process is just a cruel trick. The only difference? This “prank” isn’t funny. It can impact your health and well-being.
Understanding Prior Authorization (PA): What You Need to Know
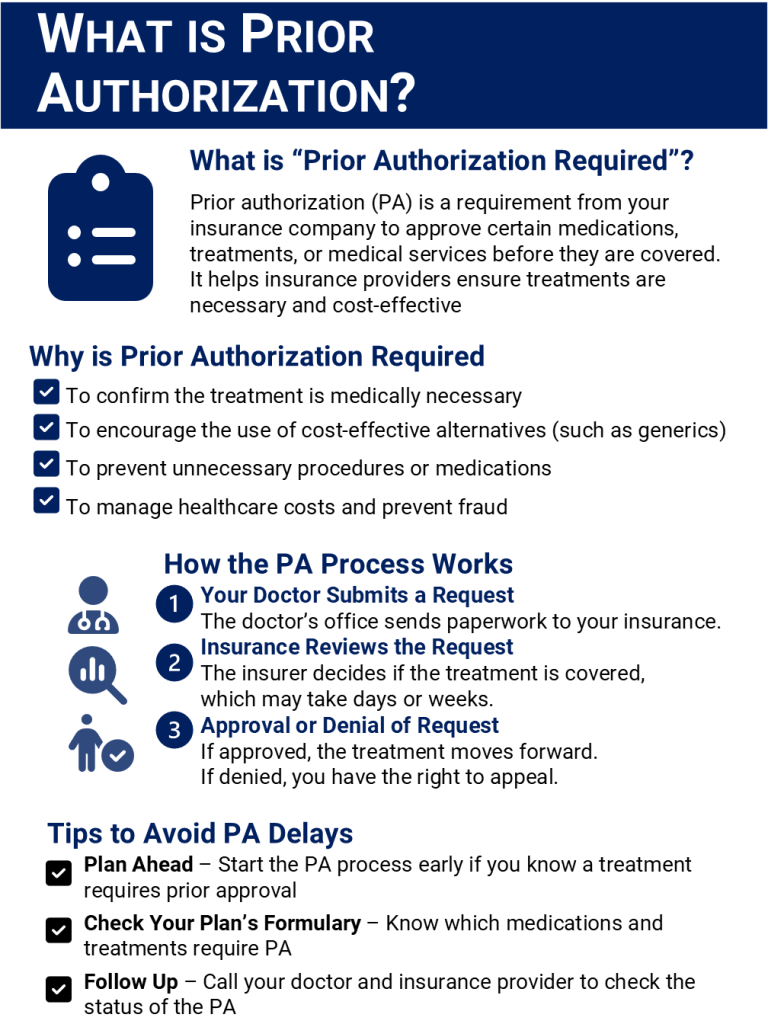
If you have ever had a prescription or medical service delayed because it needed “prior authorization,” you are not alone. Prior authorization (PA) is a common process in healthcare. When you and your doctor know you need your medication right away, it can be very frustrating. Understanding how PA works can help you navigate the system more smoothly and ensure you get the care you need without unnecessary delays.
What is Prior Authorization (PA)?
Prior authorization is a requirement of your insurance company. Certain medications, treatments, or medical services must be approved before they are covered. Essentially, you doctor must provide information to your insurance company explaining why a specific treatment is necessary.
Why Do Insurance Companies Require PA?
Insurance companies utilize the prior authorization process to:
When is PA Required?
You may need prior authorization for:
How to Handle a PA Request
If your doctor prescribes a medication or treatment that requires PA, follow these steps:
- Your Doctor’s Office Submits a Request – Your healthcare provider will send the necessary paperwork to your insurance company.
- Insurance Review – The insurance company evaluates the request. This may take days or weeks.
- Approval or Denial – If approved, you can proceed with the treatment. If denied, you have the right to appeal.
What to Do If Your PA is Denied
If your PA request is denied:
Tips for Avoiding PA Delays
Some Final Thoughts
Prior authorization can be frustrating. It is an important aspect of how insurance companies manage healthcare costs. By understanding the process and staying proactive, you can avoid unnecessary delays and ensure you receive the medications and treatments you need.
If you’ve had an experience with prior authorization (I shared a few of mine above), share your story or tips in the comments below!
